The original article can be found in: Kaieteur News By Neil Marks
Some patients who test positive for the deadly combination of Tuberculosis and HIV abruptly stop taking the prescribed medication, challenging health care workers to track them down in efforts to bring down the fatality rate.
A spike in the number of persons testing positive for the TB/HIV infection is alarming, says Dr. Jeetendra Mohanlall who runs the National Tuberculosis Programme.
Two years ago, 34 persons who tested positive for both TB and HIV died, but Dr. Mohanlall said that lives can be saved if persons stay on their medication.
“You have facilities for persons to be diagnosed, you have the treatment to give them, you have persons working with them, but they choose to default for various reasons,” Dr. Mohanlall lamented.
Last year, the National TB Programme monitored 213 cases of the TB/HIV co-infection.
For the first half of this year, of the 290 cases of TB on record, more than 60 of those persons also tested positive for HIV.
Of the co-infected patients who were recorded last year, a whopping 38 per cent defaulted on the treatment.
Patients who stop taking their medication are the biggest headache for the National Tuberculosis Programme, which is mainly responsible for monitoring patients who have the TB/HIV co-infection.
A person can be treated and cured of TB within six months. Last year, half of those who were put on treatment were cured. Those cured exclude those who dropped out of the treatment phase and those who were on continuing treatment.
Some patients stop taking the medication because of the side effects. Numbness and change in the colour of body fluids (such as urine) are two of the side effects. Patients are given vitamin supplements to deal with the numbness.
Also, some patients stopped taking the medication because of the number of pills they have to use. To avoid the so-called “pill burden” different drugs are combined into a single tablet, so patients do not have to take many tablets.
But Dr. Mohanlall said there is yet another problem in getting patients to stay on the medication. Migration is one. Some patients, he said, may move to interior regions to get into mining so as to provide for their families.
“Sometimes we plead with them to stay to complete their treatment, but they don’t all listen,” Dr. Mohanlall lamented.
To solve this problem, the National TB programme has been scurrying to meet with mining companies and mining authorities to see how best to keep the patients on treatment.
He said that the National TB Programme has been working with the Guyana Geology and Mines Commission, the country’s mines authority, but he said “we have to take that collaboration to a higher level now.”
In many cases, mining camps are located away from health care facilities, so the difficulty lies in putting patients in touch with health care workers in the regions they move to.
“Sometimes they (the patients) don’t give you any information. They just pack up and leave, and that can be a real challenge,” said Dr. Mohanlall.
He believes that families can play a major role in helping TB/HIV co-infected patients to complete their treatment.
“I’d like to recommend strong that family members support these patients. Remember they have a double disease burden to deal with, and so that may cause them to move, even if they don’t have to move to work.”
Since HIV is a virus that weakens the immune system, contracting other diseases, like TB, becomes easier.
A person can have TB infection for many years without showing any signs of TB disease; if that person’s immune system weakens, the infection can become active and develop into TB.
HIV and TB form a lethal combination, each speeding the other’s progress. Since HIV infection weakens the immune system, a person is more at risk to develop TB if exposed to the TB bacterium
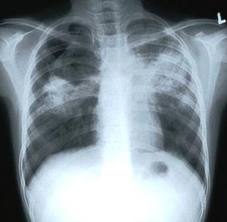
In Guyana, testing for TB is done using a Tuberculin Skin Test (TST). This screening test is done to determine whether a person who is exposed to someone with active Tuberculosis has developed latent TB infection.
A trained health care worker will inject 0.1 ml of 5 tuberculin units of purified protein derivative (PPP) into the dermis of the skin. PPD is usually administered about 2 inches below the elbow joint on the left forearm.
The TST should be read 48 to 72 hours after administration.
However, another problem faced by the National TB Programme is that some of those tested do not return, so the result is generally left unknown.
Guyana has had a collaborative programme to deal with TB/HIV infection since 2006. The country is among few countries in the world to have implemented the 12-point collaborative programme recommended by the World Health Organisation.
- Home
- News
- Views
- Opinion
- Editorial
- Features
- Clinical
- Regions
- Anguilla
- Antigua and Barbuda
- Bahamas
- Barbados
- Belize
- Bermuda
- British Virgin Islands
- Cayman Islands
- Dominica
- Grenada
- Guyana
- Jamaica
- Montserrat
- Saint Kitts and Nevis
- Saint Lucia
- Saint Martin
- Saint Vincent and the Grenadines
- Saint-Barthélemy
- Trinidad and Tobago
- Turks and Caicos Islands
- US Virgin Islands